| What is Brugada Syndrome? |
|
| Brugada Syndrome (BS) is a syndrome with specific ECG changes and a high risk of sudden cardiac death. It was first described in 1992 by Doctors Pedro and Josep Brugada in a report of 8 patients who survived recurrent episodes of sudden cardiac death. |
|
| What are the diagnostic criteria for BS? |
|
| To make a diagnosis of BS, there must be the following: |
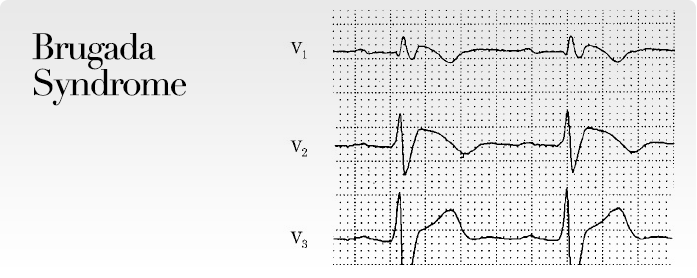
- A specific ECG pattern of right bundle branch block pattern and ST elevation in leads V1-3 (see Figure1)
- No structural heart disease on echocardiogram, angiogram, MRI or CT scan
- A history of ventricular tachycardia (VT) or ventricular fibrillation (VF), (see Figure 2) or a family history of sudden cardiac death in a first degree relative who is less than 45 years old
|
|
 |
 |
| Figure 1 |
Figure 2 |
|
|
| What conditions can mimic BS? |
- Right ventricular cardiomyopathy
- Acute myocardial infarction
- Pulmonary embolism
- Electrolytes abnormalities
- Hypothermia
- Drugs such as flecainide, procainamide and ajmaline
|
|
| How is the condition usually picked up? |
- Survivor of sudden cardiac death
- Screening of family member of a sudden cardiac death survivor
- Incidental finding during ECG screening
|
|
| What is the cause? |
|
| It is caused by a defect in the sodium channel of the cardiac cell membrane. Several genes have been discovered to cause these defects. This affects the electrical properties of the heart and makes it vulnerable to VF. |
|
| Does everyone with the ECG pattern of Brugada Syndrome have the same risk of sudden cardiac death? |
|
| No. |
|
| High risk individuals are identified by: |
- Previous history of VT or VF.
- Definite family history of sudden cardiac death
- History of syncope
|
|
| Are there any tests that can help further determine the risk? |
|
| Experts differ in their opinion on the use of electrophysiological testing in separating those at high risk from those at low risk. Electrophysiological testing is the use of electrical stimulation to test if VT or VF can be easily induced. If VT or VF is easily induced, these individuals are believed to be at higher risk. Genetic testing does not separate the high – risk from low – risk groups. |
|
| What is the treatment for BS? |
|
| In the high – risk group, implantation of a cardioverter defibrillator (ICD) is the only effective way to prevent sudden death. |
|
| In the low – risk group, electrophysiologists do not implant ICDs because of the long-term risks of having an ICD (infection, device malfunction, vein occlusion, psychological trauma). Such individuals are followed up until they show themselves to be at high risk (e.g. they develop syncope or have documented VT or VF) |
|
| Can someone with BS get better over time / Can the condition disappear over time? |
|
| Since the cause is a defect in the sodium channel, the condition cannot disappear, although the ECG changes may fluctuate over time. The ECG changes may appear just before an episode of VT/VF, during fever, or after the ingestion or infusion of certain drugs. |
|